Transforming health care: A new framework and state-of-the-art database to understand NHS and social care supply and demand
This content is AI generated, click here to find out more about Transpose™.
For terms of use click here.
The blog was co-authored by Robert King, Godspower Oboli and Ben Bray (LCP) together with Hiba Sameen and Katie Fozzard (The Health Foundation).

In the post-pandemic era, our health and social care services are facing serious challenges. With staff shortages, increasing demand on services, and growing backlogs, patients are at risk of poorer outcomes.
To diagnose these issues, we need an efficient way to assess health care supply and demand. However, the data needed to answer critical questions about NHS operations and performance remain siloed.
In response, the Health Foundation have commissioned LCP Health Analytics to carry out a two-stage project bringing together experts and key stakeholders to tackle these challenges head-on by:
- Crafting a theoretical framework. Developed to help structure theory of the relationship between health care supply and demand, and how they have shifted over time and in different areas in England. This aims to improve resource allocation and understand how service distribution affects health inequalities.
- Building a game-changing database. Integrating siloed publicly available data across supply and demand in different time periods and geographies. Unlike existing platforms, it will mainly focus on NHS activity and incorporate extensive supply side metrics including data from Office for National Statistics (ONS), UK Health Security Agency (UKHSA), and other government agencies. This scale of data collection, particularly on the supply side will be a first for researchers in England.
The framework
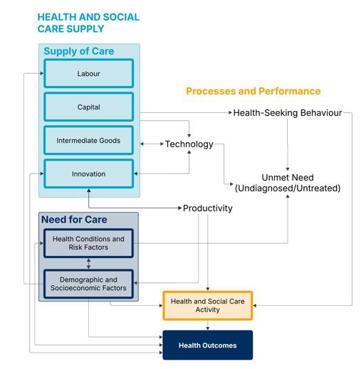
The framework is a significant step forward in understanding the complex relationships between health and care supply and demand, allowing analyses of how variations in health care resources influence service delivery and population health across England over time and geography.
The framework acknowledges the intricate balance between supply, demand, and need in health and care systems.(1) Health care differs fundamentally from traditional markets where price balances supply and demand. The NHS (a supplier) is distinct from patients (consumers). Moreover, a need for care does not always translate into demand - conditions go undiagnosed, and patients do not always seek available care. Supply side factors also operate outside conventional market forces, with elements like workforce wages set through centralised negotiations rather than market competition. This complexity means traditional methods for estimating demand and supply are not suitable in a health care setting.
Treading new ground: Supply side of the framework
The supply side of the framework may be considered the most novel. Previous research has primarily focused on demand and health outcomes, and much less on supply side factors.
Here, supply focuses on the inputs required to deliver care services. We define supply based on the ONS working definition of health care inputs as comprising the "volume estimates of labour, goods and services (intermediate inputs), and capital assets used in delivering public services. Beyond volume, we also consider the quality and unit cost of supply inputs.
The framework categorises inputs across 16 factors of production,(2) ranging from direct patient care resources (e.g. clinical staff) to supporting infrastructure (including estates and information technology) and strategic investments (e.g. education and research).
Demand and health outcomes of the framework
The demand side of the framework is built on the understanding that 'need' - the capacity to benefit from care – does not always translate into actual use of services. In the UK, where health care is free at the point of use, demand is not shaped by price but by preferences, behavioural factors and marginal costs incurred by the patient. These may include time and travel costs or any losses in productivity associated with treatment; the comparison of these costs against the marginal benefits of seeking care (most significantly, improved health) determines the quantity of health care demanded.
The framework also considers health outcomes broadly, focusing on the long-term results of care delivery at the population level. Understanding the processes and performance of the health and care system in meeting patient needs and improving population health is therefore crucial, recognising that care delivery is itself impacted by the quality, cost and volume of supply inputs measured in supply.
Processes and performance indicators capture the operational aspects of care delivery, focusing on the volume, quality, and accessibility of care across key stages of the care pathway - prevention, diagnosis, treatment, and post-treatment follow-up across the different care settings where data are available. Additionally, we also recognise the interaction between care need and health outcomes, as past care received shapes current health and influences future care needs.
A significant step forward for NHS researchers
The next phase will translate this theoretical foundation into a comprehensive database, enabling researchers and policymakers to track trends and patterns in health and care delivery. By consolidating relevant data and standardising mapping, our database will enable researchers to more easily than ever assess whether care provision meets demand and identify widening gaps.
Currently we have identified 116 supply indicators from 32 open data sources, with comprehensive coverage across the framework, and 168 demand indicators from 85 data sources including the Care Quality Commission State of Care Data, Health Survey for England, and GP Patient Survey.
The key challenge going forward is to ensure seamless analyses while accounting for variations in geographical granularity and time periods. To address this, the database will feature consistent mapping of geographical boundaries to track changes in a wide range of indicators across different areas and timeframes. The database will also include a detailed dictionary with clear mappings between data tables and the indicators within the framework, making it easier for researchers to understand the data.
Overcoming this challenge will be transformational for researchers looking to understand the supply and demand of health care in England.
Footnotes:
(1): Santana IR, Mason A, Gutacker N, Kasteridis P, Santos R, Rice N. Need, demand, supply in health care: working definitions, and their implications for defining access. Health Economics, Policy and Law. 2023 Jan;18(1):1–13.
(2): NHS Cost Inflation Index [Internet]. Personal Social Services Research Unit (PSSRU), University of Kent; Available from: https://www.pssru.ac.uk/pub/uc/uc2019/NHS-Cost-Inflation-Index.docx
Subscribe to our thinking
Get relevant insights, leading perspectives and event invitations delivered right to your inbox.
Get started to select your preferences.




