Using biomarker-based biological ages to unravel the determinants and progression of later life health
Health analytics Life sciences
On International Day of Older Persons (1 October),
LCP’s Dr Mei Chan explains why ageing is such a captivating and complex topic using her previous research findings, and how cutting-edge research in ageing and risk modelling can help us understand the determinants and progression of later life health in populations better.
Healthy ageing - how ‘health’ and ‘age’ are intertwined
Age is the strongest risk factor for most chronic diseases. The accumulation of chronic diseases over time, resulting in functional disability, frailty and multimorbidity, is well documented worldwide. However, the doubling of life expectancy in the past two centuries across high income countries, as well as the presence of inequalities in disease burden and multimorbidity, suggest that these consequences of ageing are highly modifiable. These consequences are not just attributable to a single group of diseases, but span a wide range of diseases and body systems (Table 1).
Unlike chronological age, indicators of ageing such as healthy life expectancy capture the relationship between health and ageing. The UK Government’s green paper on preventative health and its more recent Levelling Up white paper set an ambitious goal to improve healthy life expectancy by at least 5 extra years by 2035, and to close the gap between the richest and poorest areas. This is welcome, but it is a long way from the recent trend of worsening healthy life expectancy in the UK in 2008-2016, and then the devastating effect of Covid-19 on global health.
Table 1: Chronic diseases whose incidence patterns in a UK population are strongly age-related
Body system |
Disease |
|
Cardiovascular |
Cardiac arrhythmia Heart failure Ischaemic heart disease Peripheral arterial disease Stroke |
|
Musculoskeletal |
Arthritis Osteoporosis |
|
Metabolic |
Diabetes mellitus Chronic kidney disease Liver disease Gout |
|
Neurological |
Dementia Parkinson’s disease Motor neuron disease |
|
Respiratory |
Chronic obstructive pulmonary disease |
|
Inflammatory |
Rheumatoid arthritis Connective tissue disease |
|
Gut |
Diverticular disease Gall bladder disease Peptic ulcer disease |
|
(Numerous) |
Cancers |
Chronological age vs biological age – how old we are vs how old our bodies are
When analysing relationships among health outcomes (such as the onset of chronic disease and mortality) and their risk factors, chronological age is often treated as a risk factor, but it essentially captures the effects of ageing that are triggered by other risk factors not within scope in the analysis. Additionally, we cannot modify our health through modifying our chronological age. Conversely, the effects of ageing that biological risk factors, or biomarkers, such as blood pressure and BMI convey can be combined into a biological age (Figure 1). This biological age indicates how much faster or slower a person has aged compared to others, and their relative risks of poor health in later life. When these biomarkers are measured earlier in life, biological ages can capture early signs of ageing and indicate the extent to which health can be improved in individuals.
During my PhD at the University of Oxford, I estimated two main types of biological age using measurements of 72 biomarkers:
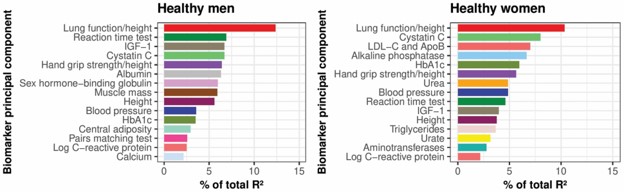
- Initially, where I prioritised biomarkers whose measurements changed most with chronological age, the most important biomarkers in biological age (in terms of the proportion of variation they explained) were reduced lung function, reduced kidney function, slower reaction time, lower insulin-like-growth factor 1 and lower hand grip strength (Figure 1).
- Subsequently, where I prioritised biomarkers that best predicted risk of onset of 20 diseases grouped into 8 body systems (similar to those in Table 1), the most important biomarkers in biological age were higher general adiposity, lower central adiposity in men and lower hand grip strength in women.
Figure 1: Key physical and biochemical biomarkers ranked by their relative importance (in terms of proportion of variation explained, R2), in a study of biological ages of healthy UK Biobank participants
Both types of estimated biological age improved predictions of later life health, including general health outcomes: mortality from chronic disease and age-related frailty. This improvement persisted after taking into account sociodemographic and health behavioural patterns. Additionally, by weighting body system ages by their predictive power of these general health outcomes in the second biological age, gut, cardiac and neurological ages for men, and musculoskeletal and neurological ages for women featured strongest.
Returning to the starting point, chronological age appears to be the strongest risk factor for most chronic diseases – as usually one or a small number of aspects of the ageing process are considered or measured in typical biomedical studies. Only when a more holistic view of ageing is assessed, in this case a wide range of biomarkers across body systems, would chronological age play less of a part in predicting later life health, and other risk factors, which can be collectively summarised into a biological age, play a greater part.
Cutting edge methods for measuring ageing
This research is an example of how high-dimensional statistical methods can be used to capture and summarise the large number of socio-demographic, behavioural and biological risk factors for each disease, and also the overall ageing process. These methods can be used to enhance the analysis of wide-ranging effects of health interventions (for example repurposing medicines to treat additional diseases) and help to inform integrated healthcare strategies across disease areas.
I also used statistical methods that track the progression of health over time and its dependency on a large number of risk factors. These methods better utilise the richness of the data in health records and population biobanks. These improve on typical epidemiological and health economic analyses, which do not normally account for the wider effects of ageing and multimorbidity on health trajectories.
Implications for healthcare and an ageing population
Analysing the ageing process in terms of individuals’ biomarker measurements earlier in life will help early detection of poorer health and increase opportunities to intervene to reduce the risk of later life disease. It also highlights biomarker-disease relationships where further research on biological mechanisms should be prioritised.
Healthcare provision and funding currently tend to be determined by a small subset of health risk factors such as chronological age, gender and geographical patterns, or one or several key biomarkers of interest. These research findings demonstrate that more recognition should be given by decision-makers to individual variation in health, across a larger range of risk factors. This would help to support two of the key tenets of the NHS Long Term Plan: personalised care and ageing well.
Indicators of healthy ageing, such as biological age, are inadvertently indicators of health inequality. Individual-level indicators can complement and provide further granularity on the determinants of health, compared to place-based, national indicators such as the ONS Health Index and healthy life expectancy statistics, if relevant data is collected in an equitable manner.
With further research, these findings can eventually support population health and life science approaches to improve and to target inequalities in healthy life expectancy.
Acknowledgements: Much of this research was conducted as part of my DPhil (PhD) in Population Health at the University of Oxford. I thank my supervisors Professor Sarah Parish, Dr Matthew Arnold and Professor Rafael Perera, and funder Nuffield Department of Population Health.

