
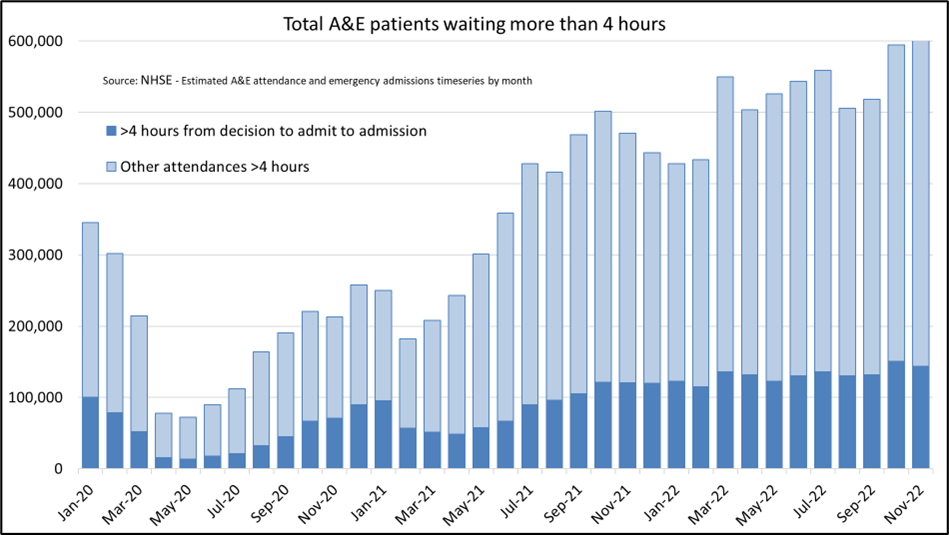
Since the summer of 2021, waiting times for admissions to accident and emergency (A&E) departments in England have been outside seasonal norms and have progressively worsened.
That being the case, it is reasonable to question if patient outcomes may be affected. Might people be dying because of delays obtaining care?
In our analysis, we estimate the number of deaths attributable to recent long waiting times. We then go on to estimate the contribution that these deaths may be making to recent “excess deaths”, by deducting the number of deaths attributable to long waiting times prior to the pandemic.
The NHS publish two measures of A&E waiting times:
- Total time spent in A&E from arrival to discharge, transfer or admission.
- Waiting time from the decision by a clinician to admit the patient and their admission (or “trolley wait”)
The chart below shows the number of people waiting more than four hours on each of these measures. The total wait time number is much larger than the “trolley wait” number because it includes time spent before a clinician made the decision to admit the patient, and it includes patients who were not ultimately admitted.
Research published in the Emergency Medical Journal and previously cited by the NHS estimated the association between delays to patient admission from the emergency department (i.e. the first of the NHS measures listed above) and all-cause 30-day mortality. This study examined the association between duration of A&E waits and the risk of dying, for over five million people admitted to hospital in England between April 2016 and March 2018, and accounted for many factors that also influence mortality risk, such as age and comorbidities.
Table 1: Effect on mortality of increasing time from patient arrival to inpatient bed transfer as shown by the standardised mortality ratio (SMR) and number needed to harm
|
Hours spent in the Emergency Department |
SMR |
Adjusted absolute mortality rate |
Number needed to harm (30-day mortality) |
|
Up to 4 hours |
0.94 |
8.2% |
-191 |
|
4-6 hours |
1.06 |
9.2% |
191 |
|
6-8 hours |
1.14 |
9.9% |
82 |
|
8-12 hours |
1.16 |
10.1% |
72 |
Source: Jones S, et al. Emerg Med J 2022; 39:168-173. doi:10.1136/emermed-2021-211572
The analysis found increased 30-day mortality for patients admitted to hospital after five hours. The 30-day mortality rate increases in an approximately linear fashion from this point until statistically significant data points are unavailable after twelve hours. It is estimated that there could be one additional death for every 82 patients waiting 6-8 hours and for every 72 patients waiting 8-12 hours.
Method
We combined the waiting time data with the published research to estimate the additional deaths associated with long delays in A&E in England. These are additional deaths compared to what we would expect if there were no long delays admitting patients.
The match between the data we have available and the research on harms arising is imperfect as we only have data showing whether waiting times exceeded four and twelve hours, whereas the research uses more granular categorisation of wait times. We have therefore estimated the excess mortality arising from long delays using two approaches. For each approach we have used data from September 2022 until the last data point available.
Trolley waits only
The chart below shows the number of patients waiting more than four hours between the decision to admit them and their admission, i.e. it does not include the period up to the decision to admit. This is broken down between those waiting four to twelve hours and those waiting twelve hours or more.
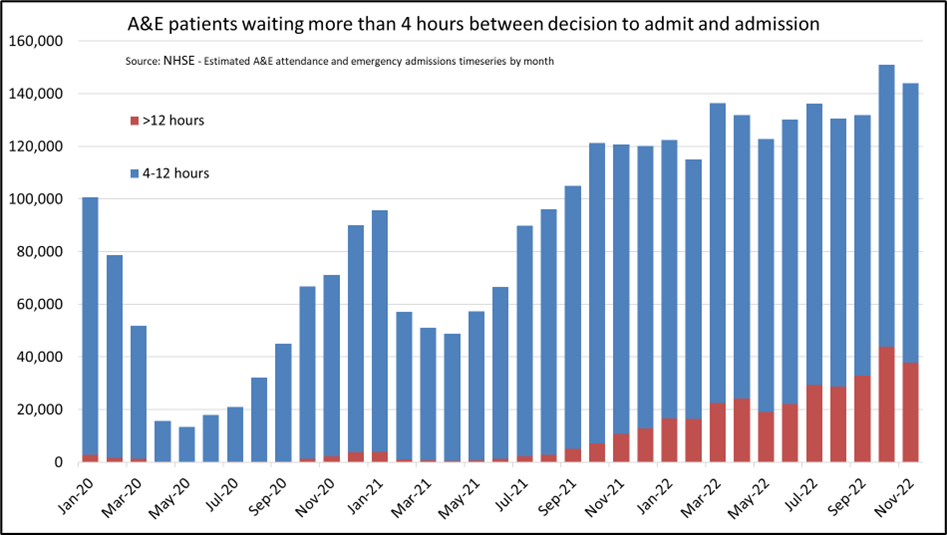
In September, October and November 2022 there were over 426,000 patients who waited more than four hours from the decision to admit. Of these, over 114,000 waited twelve hours or more.
|
Period |
Number of patients spending >4 hours from decision to admit to admission |
Number of patients spending >12 hours from decision to admit to admission |
|
September 2022 |
131,861 |
32,776 |
|
October 2022 |
150,922 |
43,792 |
|
November 2022 |
143,949 |
37,837 |
|
Total |
426,732 |
114,405 |
We estimated a lower uncertainty bound for the number of additional deaths arising from these delays by summing the two figures below:
- Additional deaths from delays of 4-12 hours, calculated by dividing the number waiting 4-12 hours by the “number needed to harm” from 4-6 hour delays (191); and
- Additional deaths from delays of more than twelve hours, calculated by dividing the number waiting twelve hours or more by the “number needed to harm” from 8-12 hour delays (72).
This results in 3,224 additional deaths in three months, or 248 each week.
This is likely be an underestimate because:
- we have made no allowance for the waiting time before the decision to admit the patient
- within the group waiting 4-12 hours, the average wait will be longer than 4-6 hours
- within the group waiting over twelve hours, the average wait must be longer than 8-12 hours
- the research found that the longer the wait the more additional deaths occur.
We then used this method to estimate a central estimate of additional deaths by taking the additional deaths occurring from mid-waiting times of the grouped data. This time we use the “number needed to harm” for 6-8 hour delays (82) for the group waiting 4-12 hours. We don’t have the distribution of waiting times for people within this group, so we assumed that the average waiting time would be in the 6-8 hour range.
This estimate results in approximately 5,398 additional deaths in three months, or 415 each week. Again, no account has been taken of the waiting time before the decision to admit and we have not allowed for extra harm arising when dates are more than twelve hours.
Total waits
The total number of A&E attendances exceeding four and twelve hours must be larger than the respective trolley waits, which are a subset of total waits. The data shows that it is considerably larger, with over 1.6 million people in major A&E departments waiting more than four hours between arrival in A&E and time of discharge, transfer or admission between September and November 2022. That compares to 426,000 with a trolley wait exceeding four hours.
The 1.6 million people waiting four hours or more, includes a significant number who waited twelve hours or more. NHSE data shows that there were over 286,000 total waits exceeding twelve hours in eight weeks in September and October.
If we divide this by the “number needed to harm” from 8-12 hour delays (72) then we get 3,976 additional deaths in eight weeks, or 497 each week.
This is an approach that we have seen elsewhere and so include as an alternative method. Importantly though, the number of total waits exceeding twelve hours includes some people who were not admitted (i.e. they were discharged or transferred). The long delay may result in adverse outcomes for these patients but applying the same “number needed to harm” as for the patients admitted is likely to overstate additional deaths.
On the other hand, this estimate may be conservative because:
- Here we have made no allowance at all for additional deaths arising from people waiting less than twelve hours. A reasonably high proportion of the 4-12 hour waits may be people who weren’t admitted so it did not seem appropriate to calculate additional deaths for these people using the “number needed to harm” for admitted patients
- We have used the published estimate “number needed to harm” for 8-12 hours waits for patients where the wait exceeded twelve hours. The research found that the longer the wait the more additional mortality arises.
Contribution to excess deaths
Our estimates above outline the number of additional deaths compared to what might have been expected if there were no long delays in A&E.
An alternative approach is to consider “excess deaths”. Excess deaths calculations typically compare mortality now to what was expected or observed in a prior period. To analyse the contribution that A&E delays may be making to excess deaths, we deduct the number of deaths arising from long delays prior to the pandemic from the number arising now. In the five years leading up to the pandemic we calculate 80 (in 2015) to 220 (in 2019) deaths arising from long delays at the same time of year using the “trolley waits” approach.
This leads to the increase in long A&E delays contributing between 200 and 340 excess deaths each week between September and November, compared to what was experienced before the pandemic. Exactly how many depends on the year or years used for the comparison.
Limitations
Our approach draws heavily on a published study showing the association between delays to patient admissions and all-cause 30-day mortality. Our conclusions therefore depend on the accuracy of that study, which was peer reviewed and has been widely cited. Our results also depend on the relationship between waiting times for admission to A&E and 30-day mortality being unchanged since the study period (2016-18). Plausibly this might have changed if the case mix of patients is different.
Conclusion
Our analysis suggests that a significant number of patients could be dying because of long delays accessing emergency care. We estimate this number at over 400 deaths each week between September and November, though it might be higher. The measure we have used is 30-day mortality, so not all of these deaths occur within A&E, or even within the hospital setting.
There have always been some long delays in A&E departments, particularly during the winter months, but the delays have grown considerably longer since the summer of 2021. This suggests that more additional deaths from long delays might be occurring than was the case pre-pandemic, so this issue is likely to be contributing to observed excess deaths. Depending on the reference period used for comparison, additional delays in A&E may be associated with between 200 and 340 excess deaths each week. Further research that provides estimates at regional and more local level would provide further insights.

